Glaucoma is a chronic eye disease that can lead to irreversible vision loss if left untreated. It occurs when the optic nerve, which connects the eye to the brain, becomes damaged. This often happens due to a buildup of pressure inside the eye, known as intraocular pressure (IOP). While there are several non-surgical treatment options available, in some cases, surgical intervention may be necessary to effectively manage glaucoma. In this article, we will explore the various surgical treatment options for glaucoma and discuss their benefits and risks.
Understanding Glaucoma
Before delving into surgical treatments, let’s first understand the basics of glaucoma symptoms and treatment. Glaucoma is often referred to as the “silent thief of sight” because it usually progresses slowly and without noticeable symptoms in its early stages. As a result, many individuals remain unaware of their condition until significant vision loss has already occurred.
The primary cause of glaucoma is an imbalance between the production and drainage of fluid in the eye, leading to increased intraocular pressure (IOP). There are two main types of glaucoma: open-angle glaucoma and angle-closure glaucoma. Open-angle glaucoma is the most common type and occurs when the drainage angle remains open but becomes less efficient over time. Angle-closure glaucoma, on the other hand, occurs when the drainage angle becomes completely blocked, causing a sudden rise in IOP.
The Basics of Glaucoma
Glaucoma affects the peripheral vision first, gradually progressing towards central vision. Common symptoms include blurred vision, halos around lights, difficulty adjusting to low light conditions, and frequent changes in glasses or contact lens prescription. Regular eye exams are essential for early detection and timely intervention.
Risk Factors and Symptoms of Glaucoma
Several risk factors increase the likelihood of developing glaucoma, including advanced age, a family history of the disease, being of African, Hispanic, or Asian descent, and certain medical conditions like diabetes. Individuals with high IOP, thin corneas, or optic nerve abnormalities are also at an increased risk.
If you experience any symptoms or fall into one or more of the high-risk categories, it is crucial to consult an ophthalmologist for a comprehensive eye examination and accurate diagnosis. Once diagnosed, your doctor will recommend an appropriate treatment plan based on the severity of your condition and the specific type of glaucoma you have.
It is important to note that glaucoma is a chronic condition that requires ongoing management. Treatment options for glaucoma include medications, laser therapy, and surgical interventions. Medications, such as eye drops, are commonly prescribed to lower IOP and prevent further damage to the optic nerve. Laser therapy, such as selective laser trabeculoplasty (SLT) or laser peripheral iridotomy (LPI), can help improve the drainage of fluid in the eye and reduce IOP. In more advanced cases, surgical interventions like trabeculectomy or glaucoma drainage devices may be necessary to control IOP.
Furthermore, lifestyle modifications can play a significant role in managing glaucoma. Regular exercise, a healthy diet, and avoiding smoking can help maintain overall eye health. Additionally, protecting your eyes from prolonged exposure to sunlight and wearing appropriate eye protection during activities that may cause eye injury are important preventive measures.
It is crucial to follow your ophthalmologist’s recommendations and attend regular follow-up appointments to monitor the progression of glaucoma and adjust the treatment plan accordingly. With early detection, proper management, and adherence to treatment, individuals with glaucoma can maintain their vision and lead fulfilling lives.
Non-Surgical Treatment Options for Glaucoma
In many cases, glaucoma can be effectively managed with non-surgical treatments. These treatments aim to reduce intraocular pressure (IOP) and slow down the progression of the disease. The two primary non-surgical treatment options for glaucoma are medications and lifestyle changes.
When it comes to medications, they are often the first line of treatment for glaucoma. They work by either reducing the production of aqueous humor, the fluid inside the eye, or increasing its drainage. Your doctor may prescribe a variety of medications to help manage your glaucoma. These can include eye drops, beta-blockers, prostaglandin analogs, carbonic anhydrase inhibitors, and alpha-adrenergic agonists. The choice of medication depends on your individual needs and medical history, so it’s important to work closely with your doctor to find the most suitable option for you.
Once you have been prescribed medication, it is crucial to follow your doctor’s instructions regarding the frequency and timing of administration. Consistent adherence to the prescribed treatment regimen is key to effectively managing glaucoma and preventing further vision loss.
In addition to medications, certain lifestyle modifications can help manage glaucoma and maintain overall eye health. Regular exercise, such as brisk walking or swimming, can improve blood flow to the optic nerve and reduce intraocular pressure. Engaging in activities that promote relaxation, such as yoga or meditation, can also be beneficial for managing stress, which can indirectly impact eye health.
Furthermore, adopting a healthy diet rich in fruits and vegetables, particularly those high in antioxidants and omega-3 fatty acids, may aid in protecting the optic nerve from damage. Some examples of these beneficial foods include leafy greens, citrus fruits, berries, and fatty fish like salmon. Additionally, it is important to limit the consumption of processed and high-sodium foods, as they can contribute to increased intraocular pressure.
Another lifestyle change that can have a positive impact on glaucoma management is smoking cessation. Smoking has been linked to an increased risk of developing glaucoma and can worsen the condition in those already diagnosed. Quitting smoking can help reduce the progression of the disease and improve overall eye health.
Lastly, it is worth mentioning that limiting caffeine intake may also be beneficial for individuals with glaucoma. While the exact relationship between caffeine and glaucoma is still being studied, some evidence suggests that excessive caffeine consumption may increase intraocular pressure in certain individuals. Therefore, it is advisable to moderate your caffeine intake and monitor its effects on your eye health.
An Overview of Surgical Treatments for Glaucoma
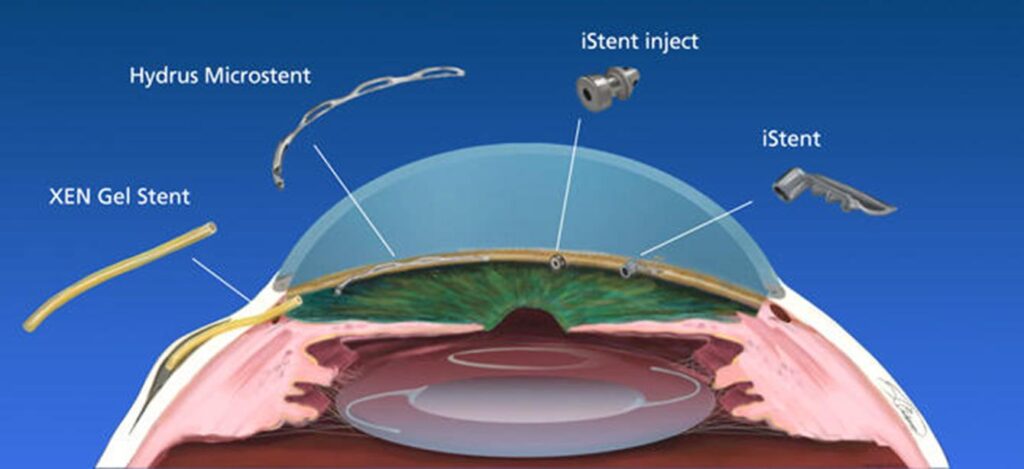
While non-surgical treatments are effective for many patients, some individuals may require surgical intervention to manage their glaucoma. Surgical options aim to improve the drainage of fluid from the eye or reduce its production, thereby lowering intraocular pressure (IOP). The choice of surgical procedure depends on various factors, such as the type and severity of glaucoma, overall eye health, and patient preferences.
When it comes to surgical treatments for glaucoma, there are two main categories: laser surgery and microsurgery. Both approaches have their benefits and risks, and your surgeon will recommend the most appropriate option based on your specific needs.
Laser Surgery for Glaucoma
Laser surgery is a common and minimally invasive treatment option for glaucoma. It involves using a highly focused beam of light to enhance the drainage of fluid from the eye. There are different types of laser surgery procedures available, each targeting specific areas of the eye to improve fluid outflow.
Trabeculoplasty is one type of laser surgery that focuses on the trabecular meshwork, the drainage system of the eye. By using laser energy, the surgeon can increase the drainage capacity of this meshwork, allowing for better fluid flow and reduced IOP.
Iridotomy, another laser surgery technique, involves creating a small hole in the iris, the colored part of the eye. This hole acts as an additional pathway for fluid to flow out of the eye, relieving pressure.
Cyclophotocoagulation is a laser surgery procedure that targets the ciliary body, which produces the fluid in the eye. By using laser energy to reduce the production of fluid, the surgeon can effectively lower the IOP.
Microsurgery for Glaucoma
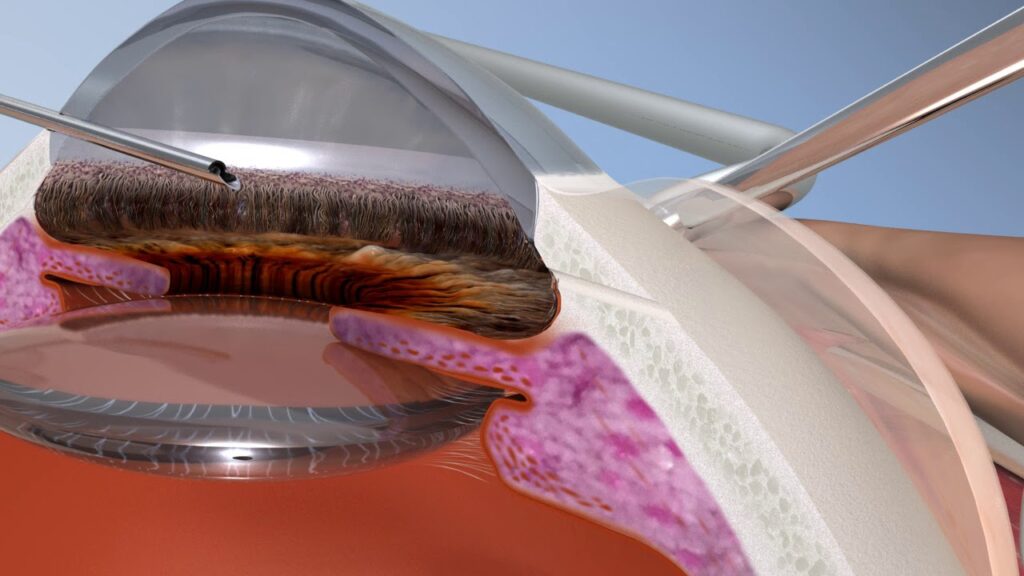
Microsurgery, also known as conventional surgery, involves creating a new drainage channel or bypass for the fluid to exit the eye. This approach is typically recommended for more advanced cases of glaucoma or when laser surgery is not suitable.
One example of microsurgery for glaucoma is trabeculectomy. During this procedure, a small flap is created in the sclera (the white part of the eye), allowing the fluid to drain out of the eye and into a small reservoir under the conjunctiva, the thin membrane covering the eye. This reservoir acts as a natural drainage system, helping to regulate the IOP.
Another microsurgical procedure is drainage implant surgery. In this technique, a small tube is inserted into the eye to create a new drainage pathway. The tube is connected to a small reservoir or plate, which helps regulate the flow of fluid out of the eye.
Both laser surgery and microsurgery have their benefits and risks. It is essential to have a detailed discussion with your surgeon to understand the potential outcomes and any potential complications associated with the surgical procedure. Your surgeon will consider factors such as your overall eye health, the severity of your glaucoma, and your personal preferences to determine the most suitable surgical approach for you.

Post-Surgery Care and Management
The recovery period after glaucoma surgery is crucial for optimal healing and long-term success. Your surgeon will provide specific instructions for post-surgery care and management. It is vital to follow these instructions diligently to minimize the risk of complications and ensure the best possible outcome.
Recovery and Rehabilitation After Glaucoma Surgery
Immediately after surgery, your eye may be covered with a protective shield. You may experience mild discomfort, redness, and watering of the eye, which should gradually subside within a few days or weeks. It is important to avoid rubbing or putting pressure on the operated eye and to refrain from any strenuous activities that can increase IOP.
Your surgeon will schedule regular follow-up visits to monitor your progress during the recovery period. They may prescribe eye drops or other medications to prevent infection and reduce inflammation.
Long-Term Management Post-Surgery
After the initial recovery period, long-term management becomes crucial to maintain the success of the surgical treatment and prevent glaucoma progression. You will need to continue regular follow-up visits with your ophthalmologist to monitor your IOP and overall eye health.
Your doctor may recommend the continued use of eye drops or other medications to control IOP and minimize the risk of complications. It is important to adhere to the prescribed treatment regimen and promptly report any changes in vision or symptoms to your doctor.
Making the Decision: Is Surgery Right for You?
Deciding whether or not to undergo glaucoma surgery is a complex decision that should be made in consultation with your ophthalmologist. The decision will depend on various factors, including the severity of your glaucoma, your vision goals, and your overall health.
Evaluating the Risks and Benefits of Surgery
Your ophthalmologist will assess the potential risks and benefits of surgery based on your specific circumstances. They will consider factors such as the success rates of surgical procedures, the likelihood of achieving your desired visual outcome, and the potential complications associated with surgery. Discussing these factors in detail will help you make an informed decision about whether surgical treatment is the right choice for you.
Discussing Your Options with Your Doctor
It is important to openly discuss your concerns, expectations, and treatment preferences with your doctor. They will provide you with all the necessary information and answer any questions you may have. Your doctor’s expertise, combined with your individual circumstances, will guide you towards the most appropriate treatment plan.
In conclusion, managing glaucoma requires a holistic approach that considers both non-surgical and surgical treatment options. While non-surgical treatments can effectively control IOP for many patients, surgical intervention may be necessary in certain cases. By understanding the basics of glaucoma, exploring non-surgical treatment options, and weighing the potential risks and benefits of surgery, you can make an informed decision about managing your glaucoma and preserving your vision. Remember to consult with your ophthalmologist to create a personalized treatment plan tailored to your needs.
Related: Types of Glaucoma Surgery and Understanding Your Choices